May 29, 2025

The article addresses the pressing need for effective strategies in behavior change within healthcare settings. It asserts that successful behavior change hinges on a multifaceted approach. This includes:
Each of these elements plays a crucial role in enhancing patient engagement and improving health outcomes. By adopting these strategies, healthcare providers can significantly elevate the quality of care they deliver.
In the rapidly evolving landscape of healthcare, the emphasis on behavior change has never been more critical. With a projected 25% increase in the demand for Board Certified Behavior Analysts (BCBAs) by 2026, the need for effective strategies to facilitate this change becomes paramount.
How are you currently addressing the challenges of hiring qualified professionals? From leveraging advanced technology to creating supportive environments and employing motivational interviewing techniques, healthcare providers must navigate a multifaceted approach to patient engagement.
This article delves into the innovative methods and frameworks that can enhance behavior change in healthcare, ultimately leading to improved patient outcomes and a healthier society.
As the industry adapts to these challenges, understanding the dynamics of behavior change is essential for both practitioners and patients alike.
Consider how Hire ABA can support your recruitment efforts and ensure you have the right talent to meet these demands.
The demand for Board Certified Behavior Analysts (BCBAs) is projected to surge by 25% by 2026, making it imperative for employers to streamline their recruitment processes. Hire ABA serves as a specialized recruitment platform that connects BCBAs with top-tier job opportunities in the field of (ABA) therapy. This platform not only simplifies the job search for BCBAs but also ensures that employers find qualified professionals who align with their organizational needs.
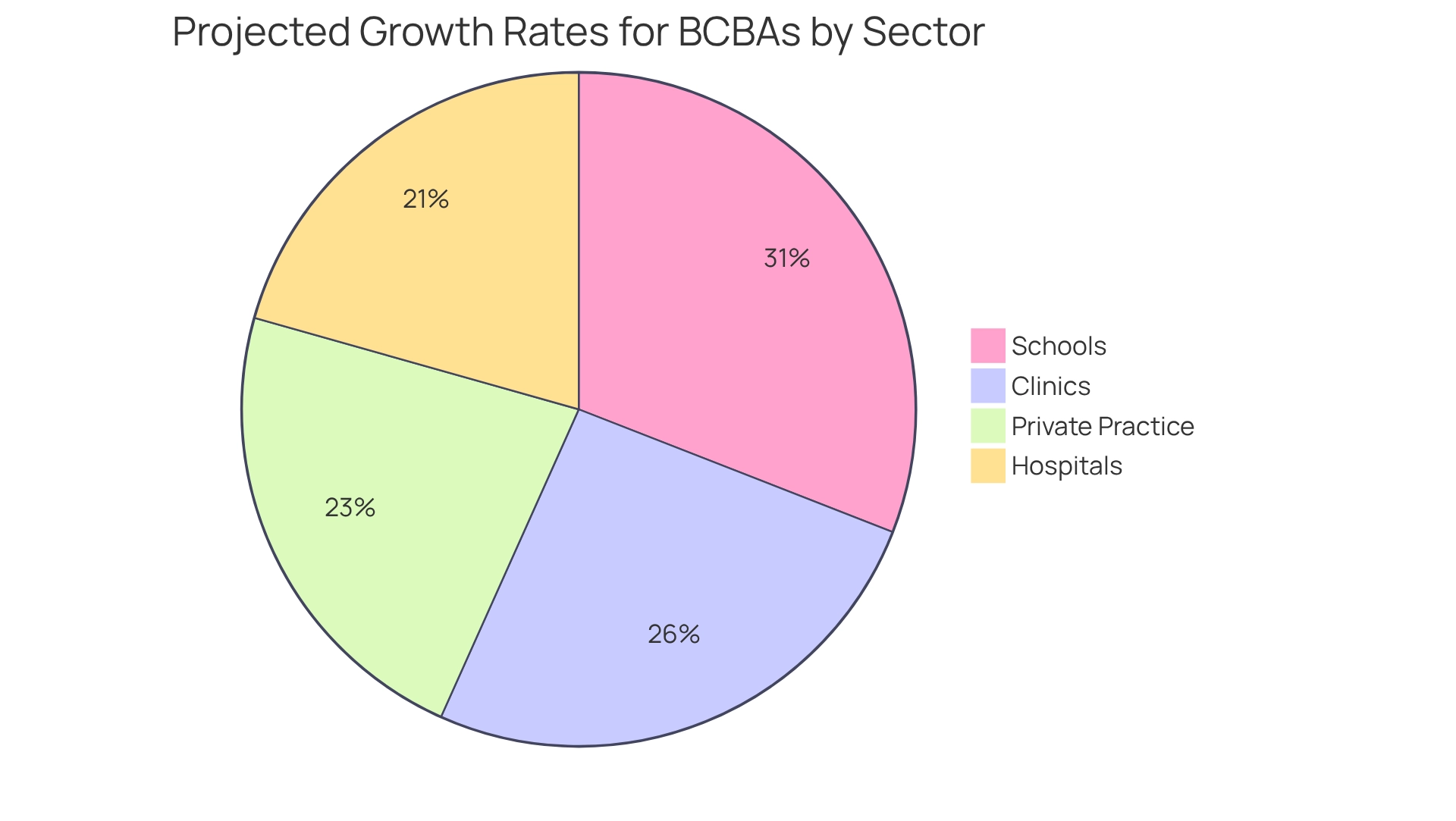
By leveraging advanced technology, including AI-driven matching algorithms and industry insights, Hire ABA enhances the recruitment experience, making it more efficient and effective for all parties involved. The job market for BCBAs is thriving, with growth rates of:
This robust demand for skilled professionals underscores the critical role of ABA in addressing behavioral requirements and promoting behavior change. As states increasingly mandate insurance plans to cover ABA services for individuals with autism, the importance of platforms like Hire ABA cannot be overstated. Are you facing challenges in finding the right talent? Hire ABA positions itself as a vital resource for employers in the medical field, helping them navigate this dynamic landscape and effectively fulfill their staffing needs. Join us in transforming the hiring process and securing the best talent in ABA therapy.
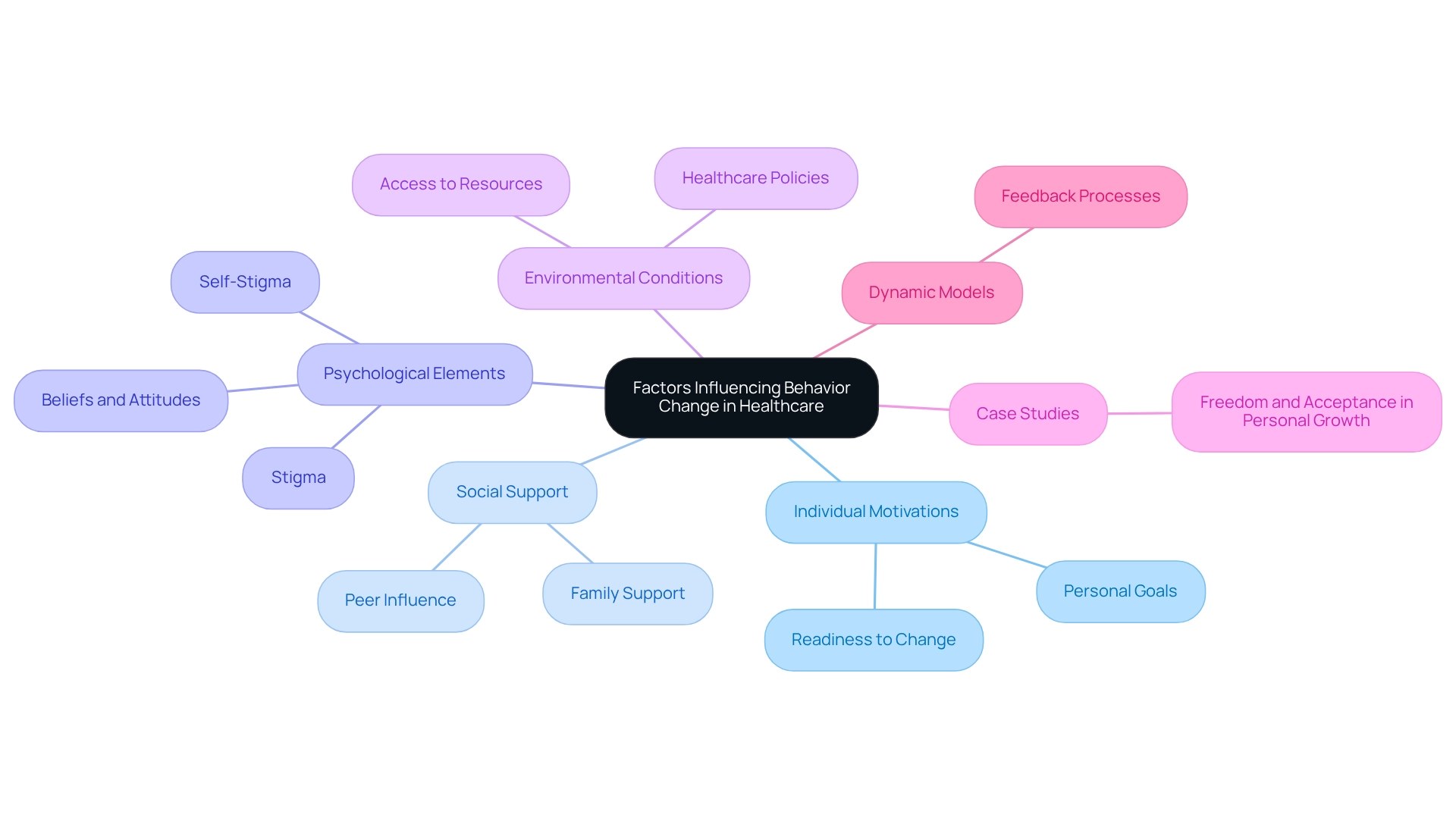
The demand for (BCBAs) is projected to increase by 25% by 2026, highlighting the urgent need for effective behavior change in healthcare strategies. Behavior change in this field is influenced by a complex interplay of factors, such as individual motivations, social support systems, and environmental conditions. Psychological elements such as beliefs, attitudes, and perceptions regarding risks to well-being significantly influence how individuals engage with wellness interventions.
For instance, research demonstrates that stigma and self-stigma represent substantial barriers to mental wellness treatment, impeding individuals' readiness to seek assistance. As noted by Peter Haugen, Aileen McCrillis, Geert Smid, and Mirjam Nijdam, 'Stigma and self-stigma are some of the most significant barriers surrounding mental health.'
Additionally, social influences, including support from family and peers, can either facilitate or hinder the process of behavior change. A notable case study titled 'Freedom and Acceptance in Personal Growth' illustrates this principle, as Skinner posited that true freedom arises from self-acceptance rather than avoidance of fears. This philosophy encourages individuals to confront their challenges, fostering personal growth and fulfillment—an essential aspect in medical environments where acceptance can lead to improved engagement with interventions.
By comprehending these dynamics, medical providers can design interventions that resonate more effectively with patients, ultimately enhancing the likelihood of successful outcomes. Moreover, dynamic models are being developed to explore feedback processes between health practices and environmental factors, providing further insights into how these elements interact. The increasing necessity for effective behavior change strategies in medical services compels providers to adapt their approaches to meet the evolving demands of the field.
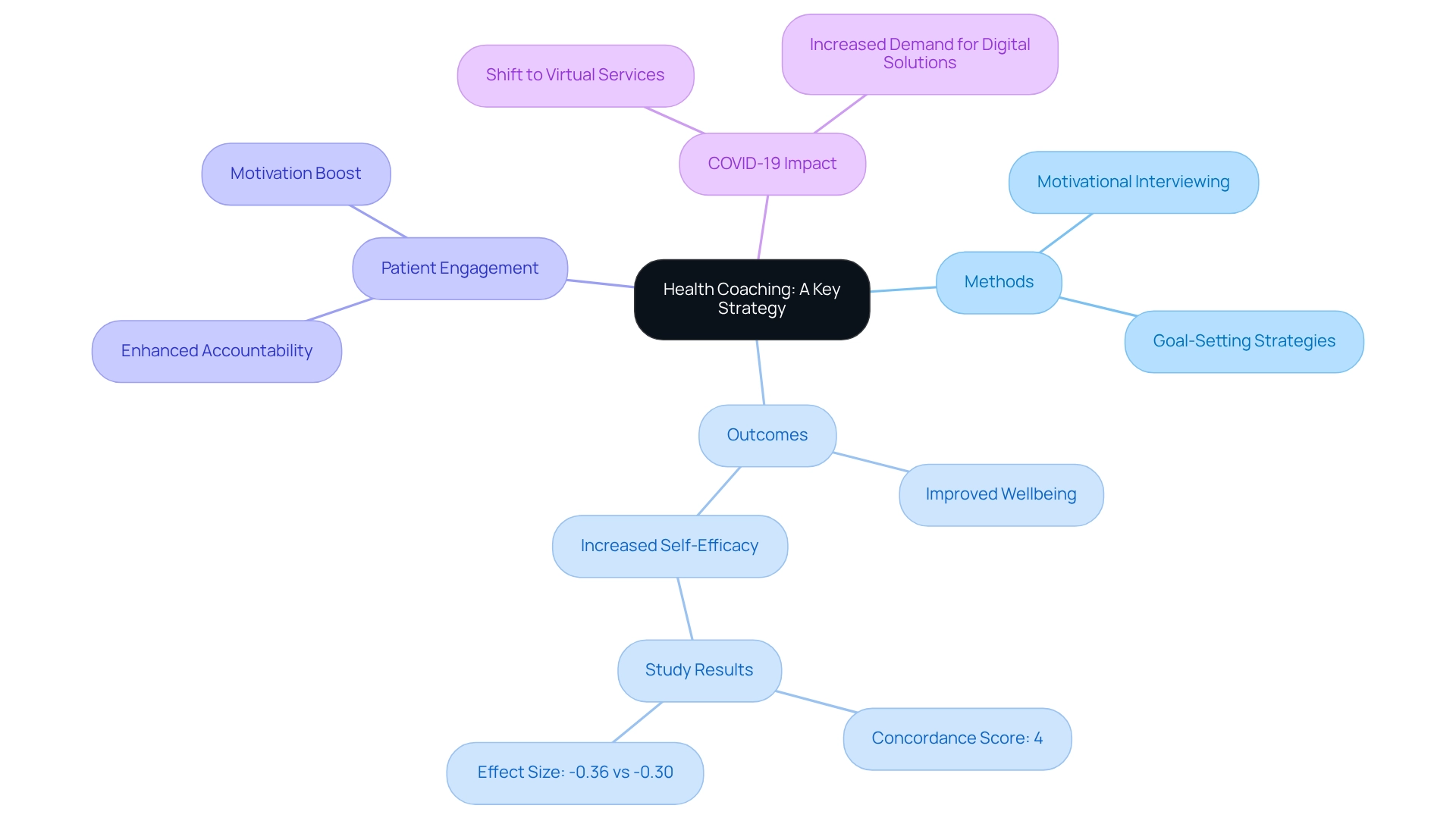
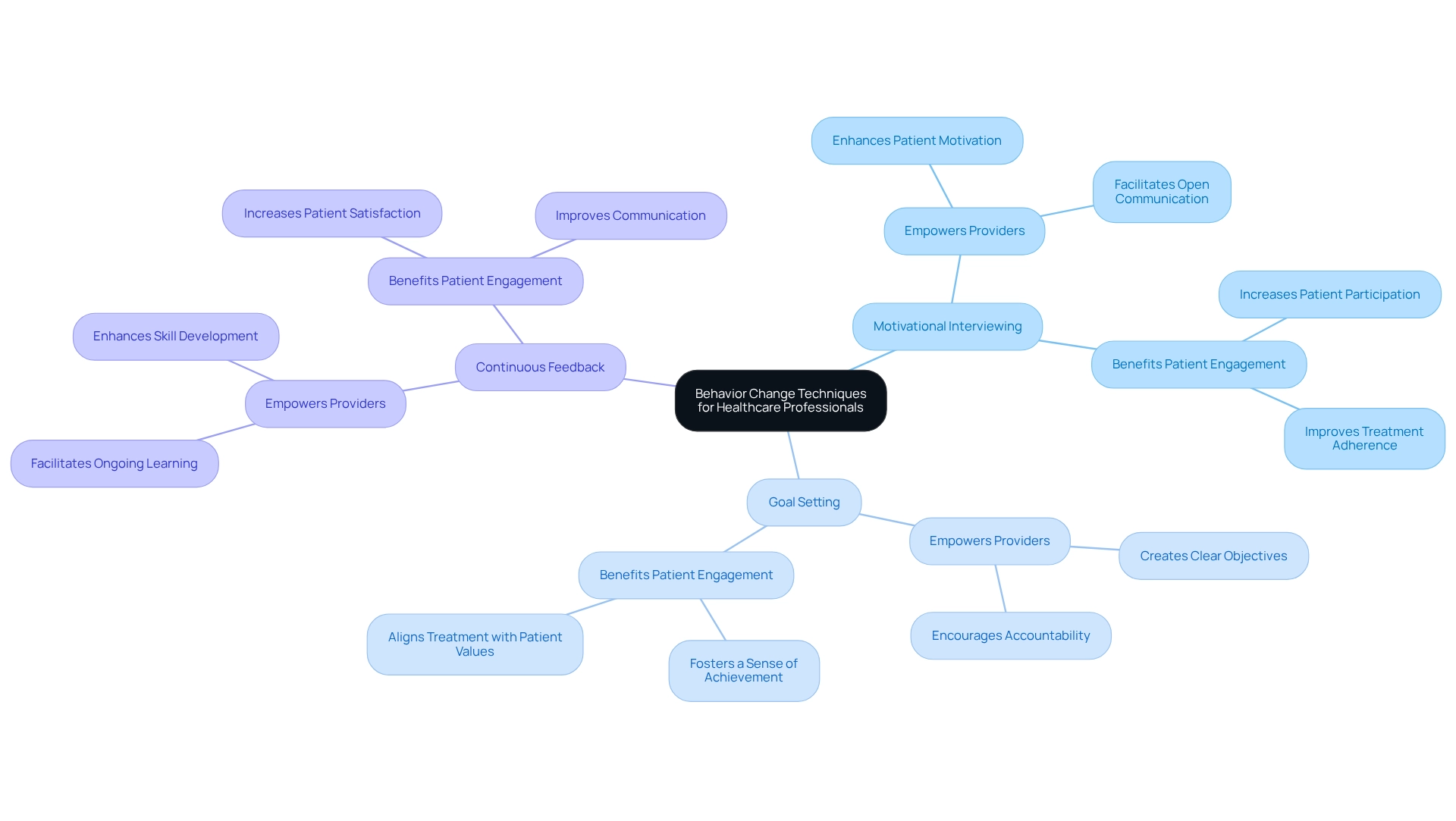
Health coaching has emerged as a vital strategy for promoting behavior change within the healthcare sector. By offering tailored assistance and direction, wellness coaches enable individuals to establish and accomplish their wellness objectives. This approach not only enhances patient engagement but also fosters accountability and motivation. Wellness coaches employ a variety of methods, including motivational interviewing and goal-setting strategies, to assist clients in navigating their wellness journeys.
Studies show that effective wellness coaching can lead to improved wellbeing outcomes, making it a crucial element of contemporary medical practices. A thorough examination of eight randomized controlled trials indicated a statistically significant influence of wellness coaching on self-efficacy among individuals with chronic conditions, with a concordance score of 4 demonstrating an effect size of -0.36 compared to -0.30 for inactive comparators. This underscores the efficacy of wellness coaching in boosting individuals' confidence in overseeing their well-being.
Furthermore, the COVID-19 pandemic has hastened the transition towards virtual medical services, further reinforcing the role of coaching in contemporary healthcare. As the demand for digital wellness solutions continues to rise, wellness coaching remains essential in fostering behavior change, ultimately resulting in enhanced outcomes for patients. As Karen Lamb wisely remarked, "A year from now, you will wish you had begun today," highlighting the significance of taking action in wellness coaching. For ongoing updates and insights into wellness coaching and related fields, can be a valuable resource.
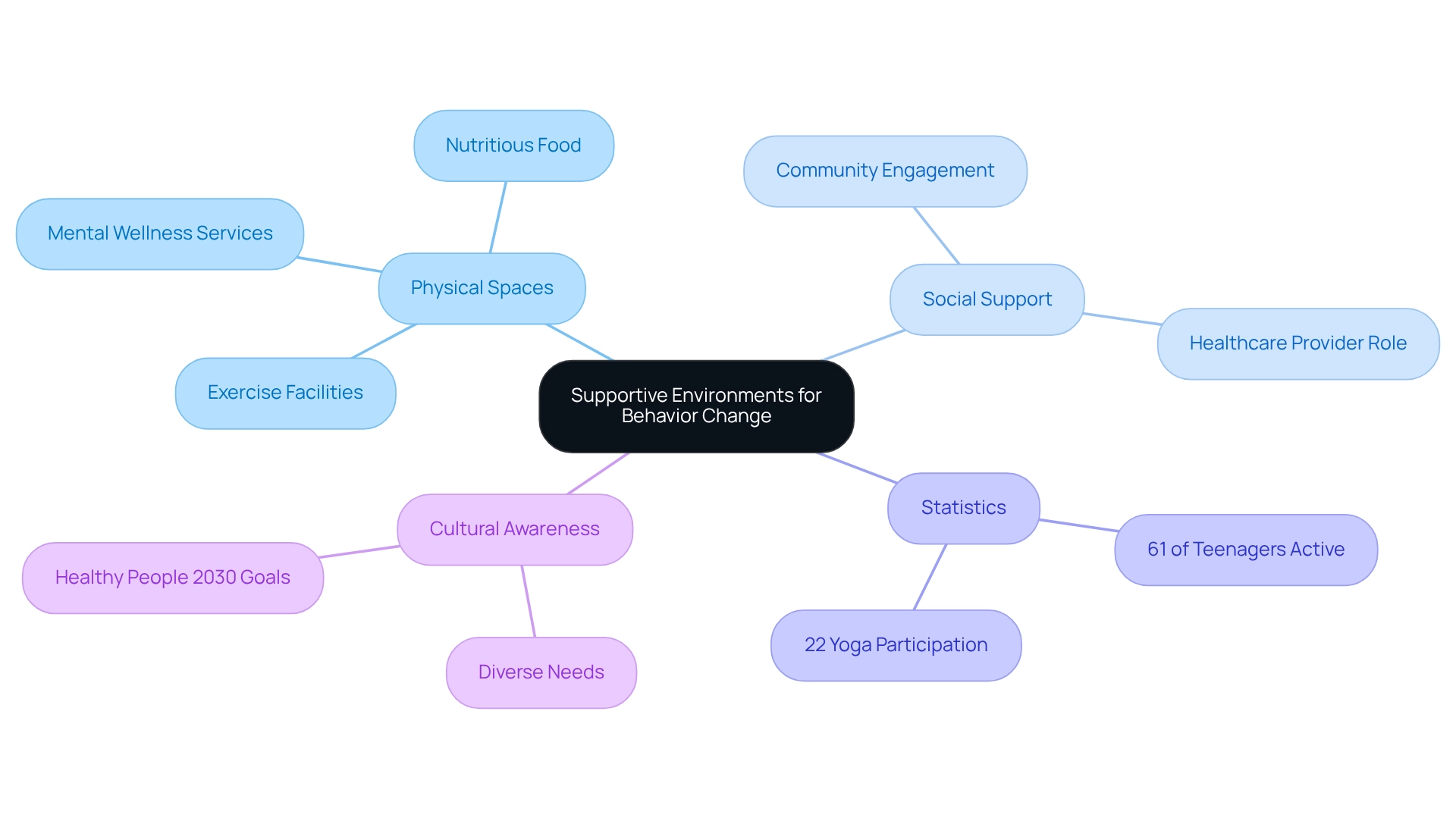
Creating supportive environments is crucial for facilitating effective behavior change. This involves not only designing physical spaces that encourage healthy choices but also establishing robust social and emotional support systems. Healthcare providers can enhance these environments by ensuring access to vital resources, such as nutritious food options, exercise facilities, and mental wellness services. For instance, studies reveal that 61% of teenagers who engage in regular physical activity report improved mental well-being. This underscores the importance of promoting active lifestyles within medical settings. Additionally, with 22% of teenagers participating in yoga over the past year, it is essential to advocate for diverse forms of physical activity as part of a comprehensive approach to well-being.
Furthermore, fostering a culture of support and understanding can significantly influence individuals' willingness to engage in behavior change towards healthier habits. As B.J. Fogg aptly states, "Make your habits invisible and automatic," emphasizing the need to create environments that facilitate effortless engagement in healthy practices. Healthy People 2030 highlights the necessity for national goals aimed at enhancing children's mental wellness and overall well-being. This can be achieved through supportive medical settings that are culturally aware and responsive to the diverse needs of the population, projected to consist of of color by 2050. By addressing both environmental and social factors, medical professionals can substantially improve the effectiveness of health interventions, ultimately leading to better outcomes for individuals and a healthier population.
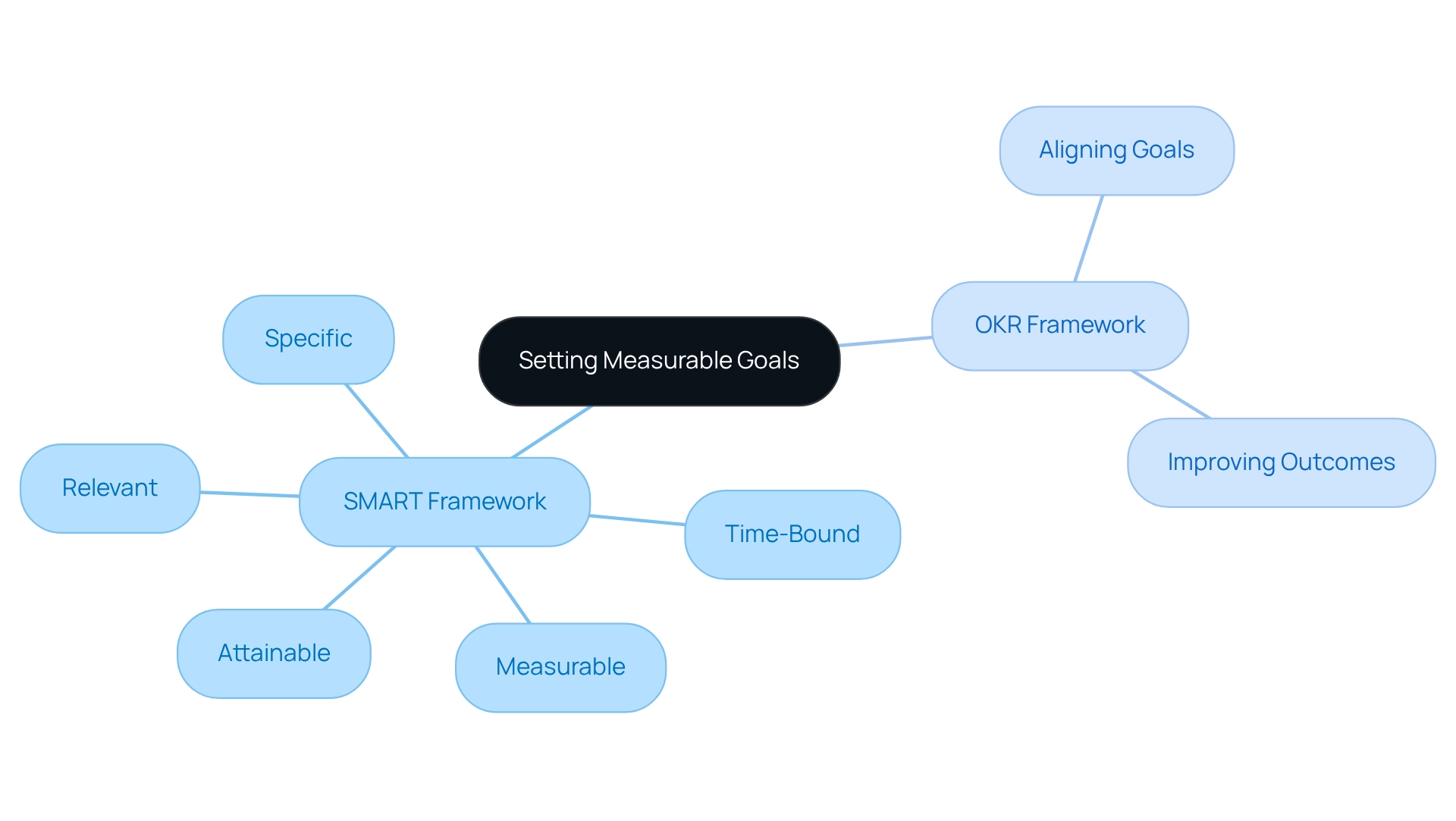
Establishing quantifiable objectives is crucial for promoting behavior change in healthcare settings. Did you know that utilizing the SMART framework—specific, measurable, attainable, relevant, and time-bound—can significantly enhance the clarity of one's objectives? This approach not only delineates a clear path toward achievement but also fosters accountability. For example, instead of like 'eat healthier,' a more effective measurable goal would be 'consume at least five servings of fruits and vegetables daily.' This specificity not only assists in tracking progress but also enables medical providers to help individuals monitor their achievements and adjust strategies as needed.
Research indicates that 83% of companies recommend the OKR framework for aligning company goals and improving outcomes, underscoring the effectiveness of structured goal-setting in enhancing results. Moreover, case studies reveal that active participation in goal-setting boosts commitment and innovation, ultimately leading to improved wellness outcomes. For instance, involving employees in the goal-setting process has been shown to increase their commitment to organizational objectives. By nurturing a sense of achievement through clear benchmarks, medical professionals can significantly enhance individual motivation and commitment to wellness objectives.
To execute this successfully, medical providers should motivate individuals to establish their own SMART objectives. This ensures a sense of ownership and involvement in their health journey, paving the way for lasting behavior change.
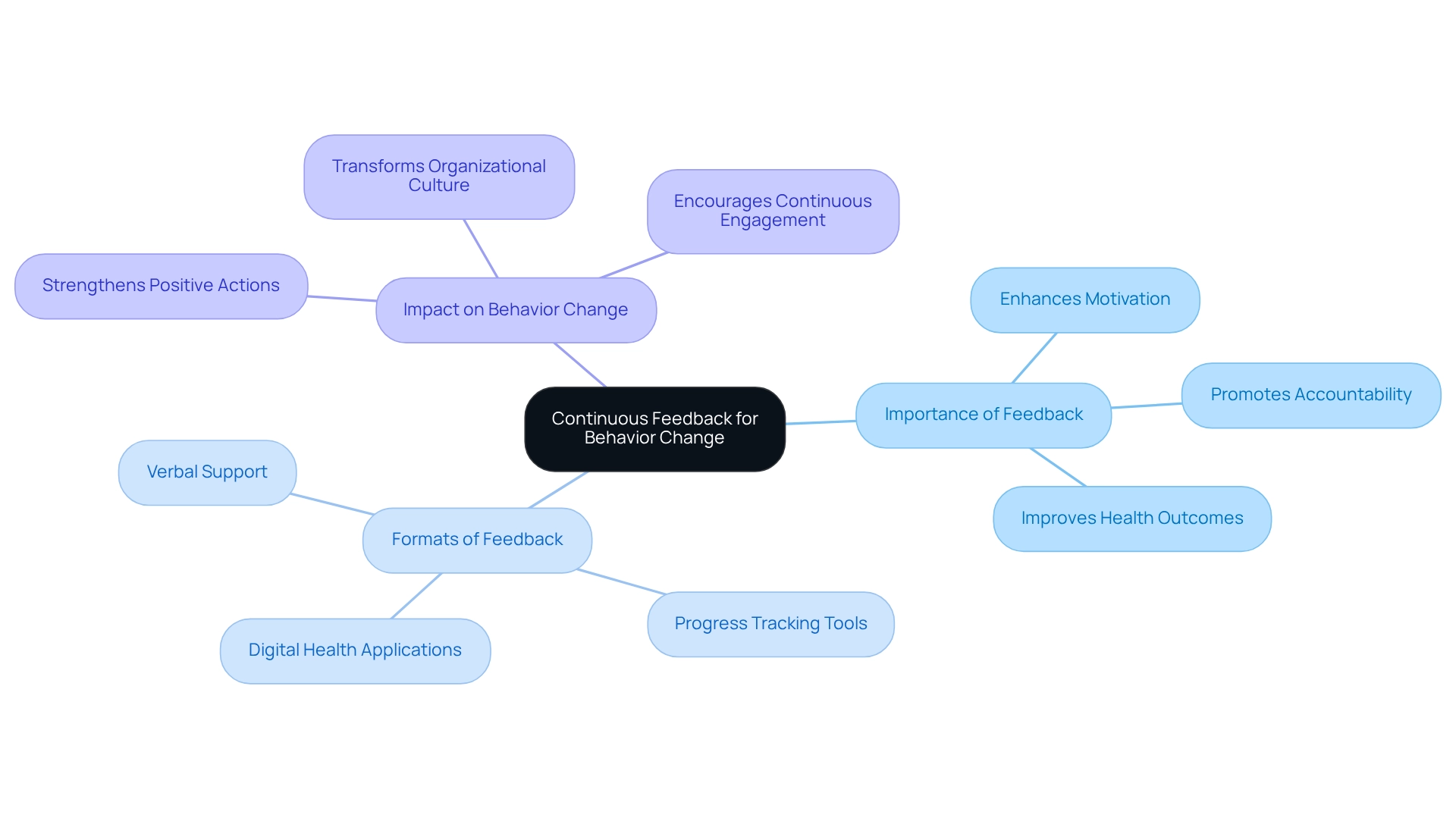
The demand for Board Certified Behavior Analysts (BCBAs) is projected to rise by 25% by 2026, underscoring the urgent need for effective change strategies in medical environments. Ongoing feedback plays a crucial role in sustaining behavior change over time. By delivering regular and constructive feedback, healthcare providers empower patients to recognize their progress and pinpoint areas needing improvement. This feedback can manifest in various formats, such as:
Research demonstrates that prompt feedback significantly strengthens positive actions, promoting accountability and dedication to personal goals. Organizations are increasingly adapting their feedback mechanisms to prioritize technology and continuous engagement. The case study " for 2024" highlights how these adaptations enhance workplace culture and overall performance. By incorporating ongoing feedback into care plans, healthcare providers can greatly enhance individual motivation and commitment to behavior change, ultimately resulting in better health outcomes.
As Nelson Mandela wisely stated, "What counts in life is not the mere fact that we have lived. It is what difference we have made to the lives of others that will determine the significance of the life we lead." This emphasizes the importance of constructive feedback in creating a substantial impact on individuals' lives.
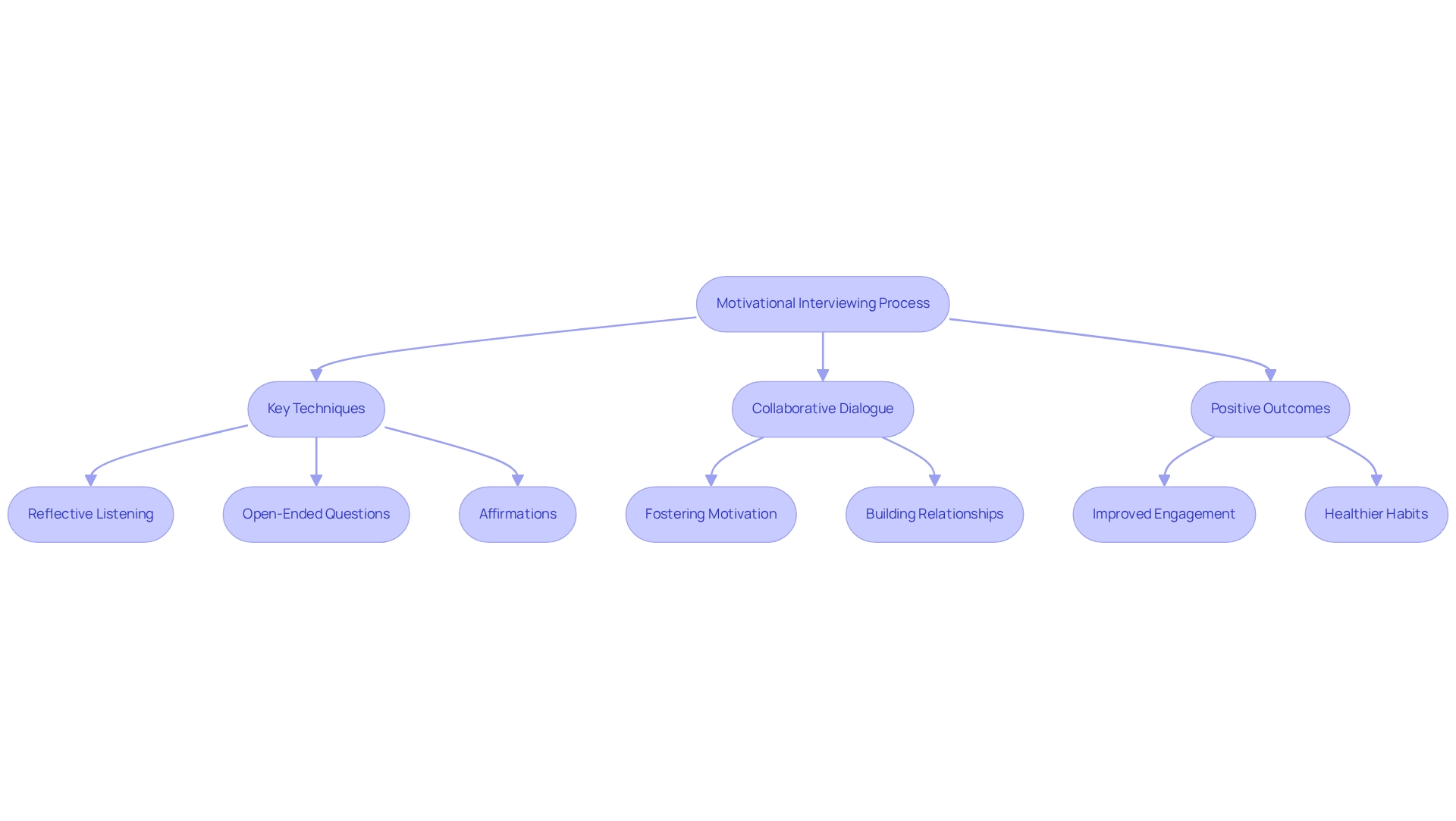
Motivational interviewing (MI) stands as a transformative technique, meticulously designed to enhance individual engagement in behavior change. This patient-centered approach empowers individuals to explore their motivations and ambivalence surrounding change. By fostering a collaborative conversation, healthcare providers can assist individuals in articulating their objectives and identifying barriers to achieving them. Key techniques, including reflective listening, open-ended questions, and affirmations, play an indispensable role in this process.
Recent studies underscore MI's positive outcomes across various health issues, highlighting its efficacy in improving individual results. For instance, a recent randomized controlled trial revealed that adolescents engaged in an MI intervention reported significantly earlier bedtimes during school days (p = 0.004), illustrating the technique's impact on habit modification. Furthermore, a study indicated that the recognition of triggers associated with recovery plans surged from 52% to 94% within the MI intervention group, showcasing the method's ability to enhance participant engagement and commitment.
The advantages of collaborative dialogue in facilitating behavior change are profound. MI not only elevates motivation but also fosters a collaborative spirit between individuals and providers, which is essential for achieving behavior change and successful outcomes. As evidenced by titled "Compassionate Engagement in Healthcare," practitioners' ability to convey genuine care—regardless of the medium—can significantly amplify the effectiveness of interventions. To implement MI effectively, medical providers should contemplate interdisciplinary approaches in lifestyle medicine, as collaboration can further enrich the individual's experience. Overall, motivational interviewing is recognized as a crucial instrument in medical care, facilitating significant behavior change and improving outcomes for individuals. Practitioners are encouraged to consistently incorporate reflective listening and open-ended questions in their interactions to optimize client engagement.
Training medical specialists on modification strategies is essential for improving client results. With a projected rise of 25% in the by 2026, the need for skilled professionals in this area has never been more critical. Training programs must prioritize evidence-based strategies such as:
These methods empower providers to assist patients more effectively in their change journeys, ultimately enhancing the quality of care.
Continuous education and professional growth are vital for providers to stay updated on the latest research and optimal methods in behavior change strategies. For instance, a research study titled "Behavioural Expectations for Health Conversations," conducted by a collaborative group from various organizations, revealed that participants rated their expectations for engaging in wellness discussions with service users at an average of 6.26 out of 10. This finding underscores the varying levels of confidence among staff, highlighting the need for targeted training programs that can elevate their capabilities. As noted by Lancashire Care Trust, while they supported module development and provided it as freely available staff training, their involvement in the study was limited, emphasizing the importance of independent research in shaping effective training.
By investing in comprehensive training initiatives, medical organizations can enhance client engagement and adherence, leading to improved health outcomes. The significance of instructing medical professionals on behavior change cannot be overstated; it lays the groundwork for effective interventions and supports the overarching goal of enhancing care for individuals. To implement effective training programs, employers in the medical field should consider integrating ongoing assessments and feedback mechanisms, ensuring that staff are equipped with the necessary skills to engage effectively with individuals.
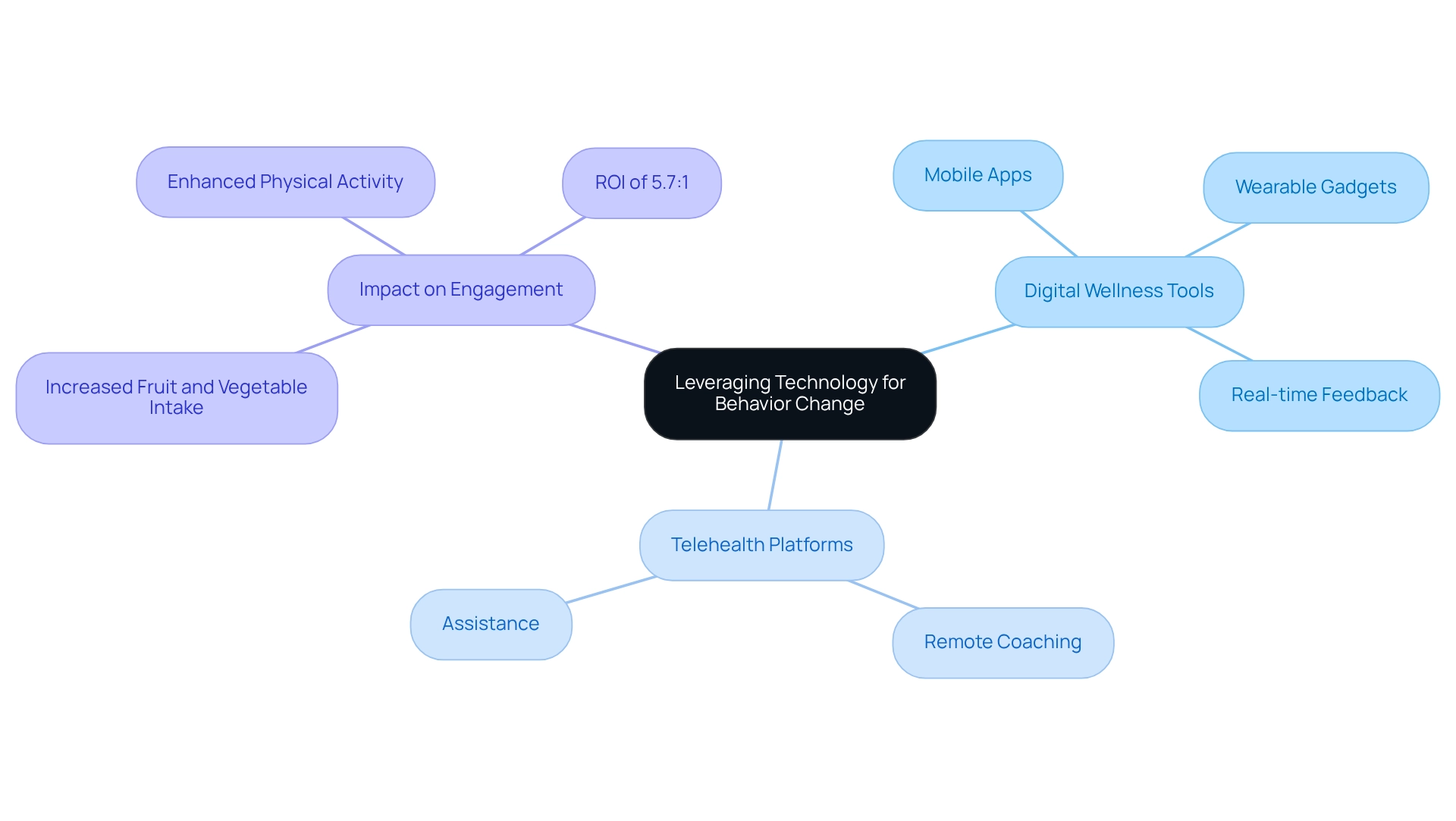
Leveraging technology is essential for implementing effective strategies for behavior change in healthcare. Digital wellness tools, such as mobile apps and wearable gadgets, empower individuals by delivering real-time feedback, monitoring progress, and offering tailored suggestions. These innovations significantly enhance patient involvement, making wellness management more interactive and accessible. For instance, a study evaluating overall wellness enhancements identified notable increases in fruit and vegetable intake and physical activity among participants, suggesting the effectiveness of customized interventions, such as text messaging, in overcoming barriers to engagement in wellness programs.
Telehealth platforms further expand the reach of medical providers, enabling remote coaching and assistance across diverse settings. By incorporating technology into lifestyle behavior change initiatives, healthcare experts can not only enhance adherence but also empower individuals to take control of their well-being. Organizations utilizing these digital tools have reported impressive , with some achieving ROIs as high as 5.7:1. As Google Health indicates, "We believe that AI is ready to change medicine, providing new, assistive technologies that will enable doctors to better support those they care for."
As we approach 2025, the ongoing development of digital wellness tools will play a crucial role in shaping effective strategies for behavior change, ultimately improving care and outcomes. Healthcare employers should consider implementing these technologies to foster better client engagement and enhance overall health outcomes.
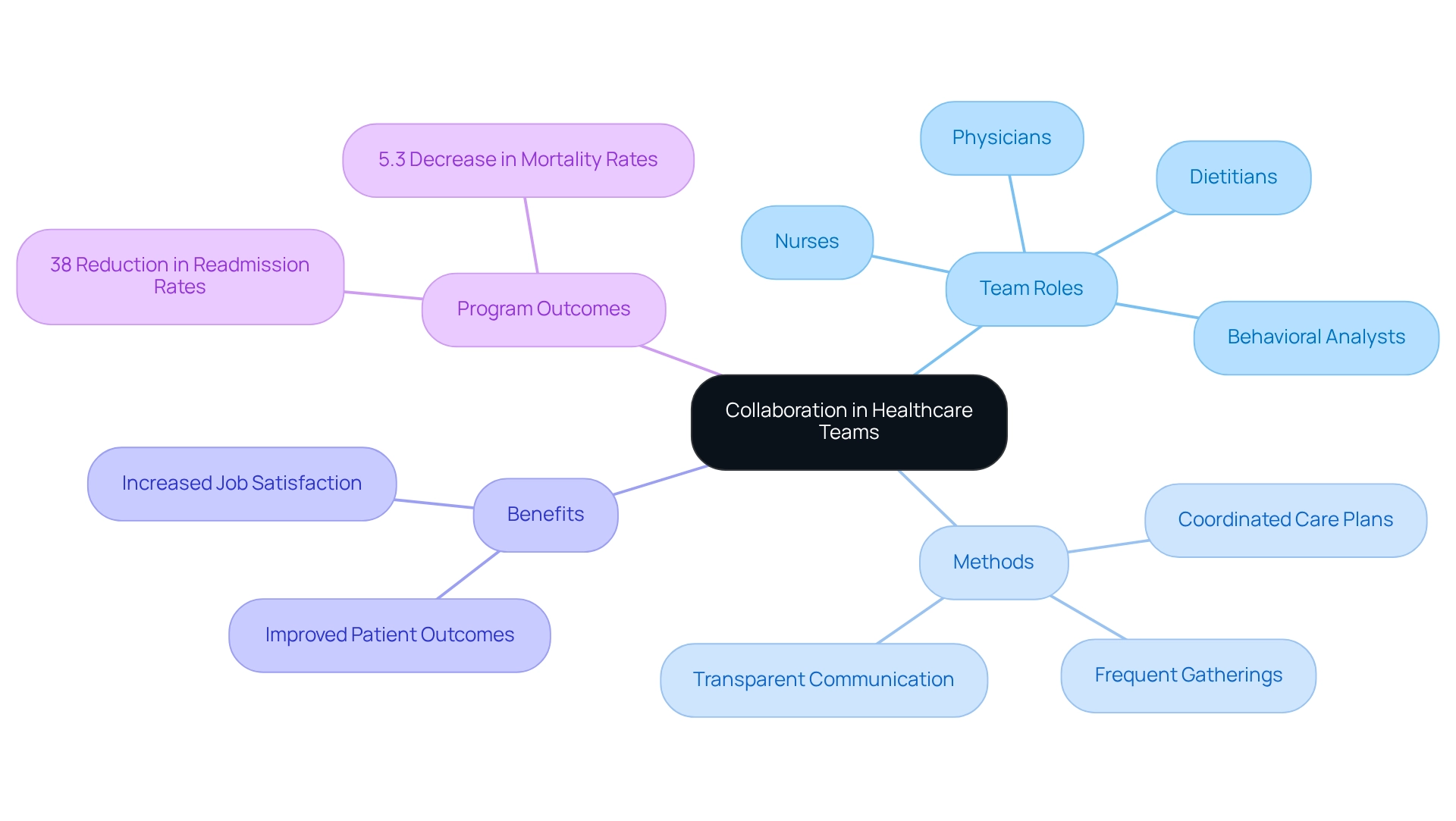
Encouraging cooperation among medical teams is vital for promoting effective change in actions. Interdisciplinary methods that involve a diverse array of professionals—including physicians, nurses, dietitians, and behavioral analysts—provide extensive assistance customized to individuals' needs.
As Littlechild noted, "Cooperation in interdisciplinary teams increases productivity, contributes to the better use of team members’ skills and leads to a greater feeling of individual responsibility for achieving the objective."
By collaborating, medical teams can:
Frequent team gatherings, common goals, and transparent communication channels are essential for improving collaboration, ensuring that all members are aligned in their efforts to assist individuals. This collaborative framework not only results in enhanced outcomes for individuals but also increases job satisfaction among medical providers.
The essential nature of interdisciplinary cooperation for improving the quality of patient care is underscored by the at Penobscot Community Health Care, which demonstrated the effectiveness of such teamwork, achieving a 38% reduction in hospital readmission rates and a 5.3% decrease in mortality rates within the first year. These outcomes highlight the significant benefits of interdisciplinary collaboration in healthcare settings.
The landscape of healthcare is shifting, with a projected 25% increase in demand for Board Certified Behavior Analysts (BCBAs) by 2026. This statistic underscores the critical importance of behavior change in improving patient outcomes. To navigate the complexities of behavior modification, healthcare providers must adopt innovative strategies. This includes understanding the factors influencing behavior change and implementing effective techniques such as:
By doing so, we can enhance patient engagement significantly.
Creating supportive environments and leveraging technology are equally vital in fostering behavior change. By ensuring access to resources and utilizing digital tools, healthcare professionals can empower patients to take control of their health journeys. Continuous feedback and interdisciplinary collaboration further enhance the effectiveness of interventions, leading to better health outcomes and increased patient satisfaction.
Ultimately, integrating these strategies not only addresses the immediate needs of patients but also cultivates a healthier society. As healthcare continues to evolve, the emphasis on behavior change remains paramount, highlighting the need for skilled professionals and effective recruitment solutions like Hire ABA. Are you facing challenges in hiring the right talent? Embracing these approaches will pave the way for improved patient care and a more robust healthcare system, reinforcing the idea that meaningful change is possible when the right strategies and support systems are in place.
What is the projected demand for Board Certified Behavior Analysts (BCBAs) by 2026?
The demand for BCBAs is projected to surge by 25% by 2026.
How does Hire ABA assist in the recruitment of BCBAs?
Hire ABA serves as a specialized recruitment platform that connects BCBAs with top-tier job opportunities in the field of Applied Behavior Analysis (ABA) therapy, simplifying the job search for BCBAs and helping employers find qualified professionals.
What technology does Hire ABA utilize to enhance the recruitment experience?
Hire ABA leverages advanced technology, including AI-driven matching algorithms and industry insights, to make the recruitment process more efficient and effective for all parties involved.
What are the growth rates for BCBAs in various sectors?
The growth rates for BCBAs are as follows: 1. 30% in schools 2. 25% in clinics 3. 20% in hospitals 4. 22% in private practice.
Why is the demand for BCBAs significant in healthcare?
The robust demand for skilled professionals underscores the critical role of ABA in addressing behavioral requirements and promoting behavior change, especially as states mandate insurance plans to cover ABA services for individuals with autism.
What challenges do employers face in finding qualified BCBAs?
Employers in the medical field may face challenges in navigating the dynamic landscape of staffing needs, which makes platforms like Hire ABA vital resources for effectively fulfilling these needs.
Our expert recruitment strategies and AI-driven sourcing ensure that you receive top-notch candidates quickly, without compromising on quality. Whether you’re looking for BCBAs, Clinical Directors, or RBTs, we’ve got you covered.