September 3, 2025

The key differences between 'behavior' and 'behaviour' lie in their usage in American and British English, respectively. Understanding these distinctions is not merely a matter of spelling; it plays a crucial role in effective communication within healthcare settings. Misunderstandings in clinical documentation can have significant implications for patient care and professionalism. Therefore, it is imperative for healthcare employers to grasp these variations to avoid potential pitfalls.
In the realm of healthcare, the nuances of language possess profound implications for patient care and professional communication. The distinction between 'behavior' and 'behaviour' transcends mere spelling; it reflects deeper cultural and contextual differences that can lead to misunderstandings in medical documentation and interactions. As healthcare continues to globalize, the challenge lies in bridging these linguistic divides to ensure clarity and enhance patient outcomes.
How can healthcare professionals effectively navigate these variations to foster better communication and understanding among diverse populations?
American English and British English, while fundamentally similar, exhibit significant differences in spelling, vocabulary, and usage that can profoundly impact medical contexts. Consider the spelling of 'color' in American English versus 'colour' in British English—this simple variation exemplifies a common discrepancy that can lead to misunderstandings if not adequately addressed. In discussing documentation, a British healthcare professional might use 'behaviour,' whereas their American counterpart would refer to it as 'behavior vs behaviour.' Linguists emphasize that even minor variations can result in considerable misinterpretations in medical documentation, potentially affecting care outcomes.
Recent studies reveal that low-income Americans face , such as diabetes and hypertension, exacerbated by communication barriers. Consequently, awareness and adaptation to these linguistic differences are crucial in a globalized medical setting to ensure clarity and effectiveness in patient care. How can we navigate these challenges? Integrating insights from linguistics specialists can illuminate the obstacles medical professionals encounter in managing these communication differences, ultimately enhancing patient results.
In light of this, it is essential to prioritize understanding and addressing these variations to improve healthcare delivery and patient outcomes.
The terms 'behavior vs behaviour' denote the same concept—observable actions performed by individuals—yet their spelling varies based on regional language preferences. 'Behavior vs behaviour' highlights that 'behavior' is the variant used in American English, whereas 'behaviour' is the variant in British English. This distinction extends beyond mere academic interest; in medical settings, the choice of spelling can significantly influence the perception of professionalism and attention to detail.
For instance, a research paper published in a British journal would appropriately use 'behaviour,' whereas an American journal would favor 'behavior,' illustrating the difference of behavior vs behaviour. Such variations are essential for medical employers to identify, as they can impact how clinical documentation is viewed and the overall professionalism expressed in interactions. Understanding these subtleties is crucial for and fostering effective interactions in diverse medical environments.
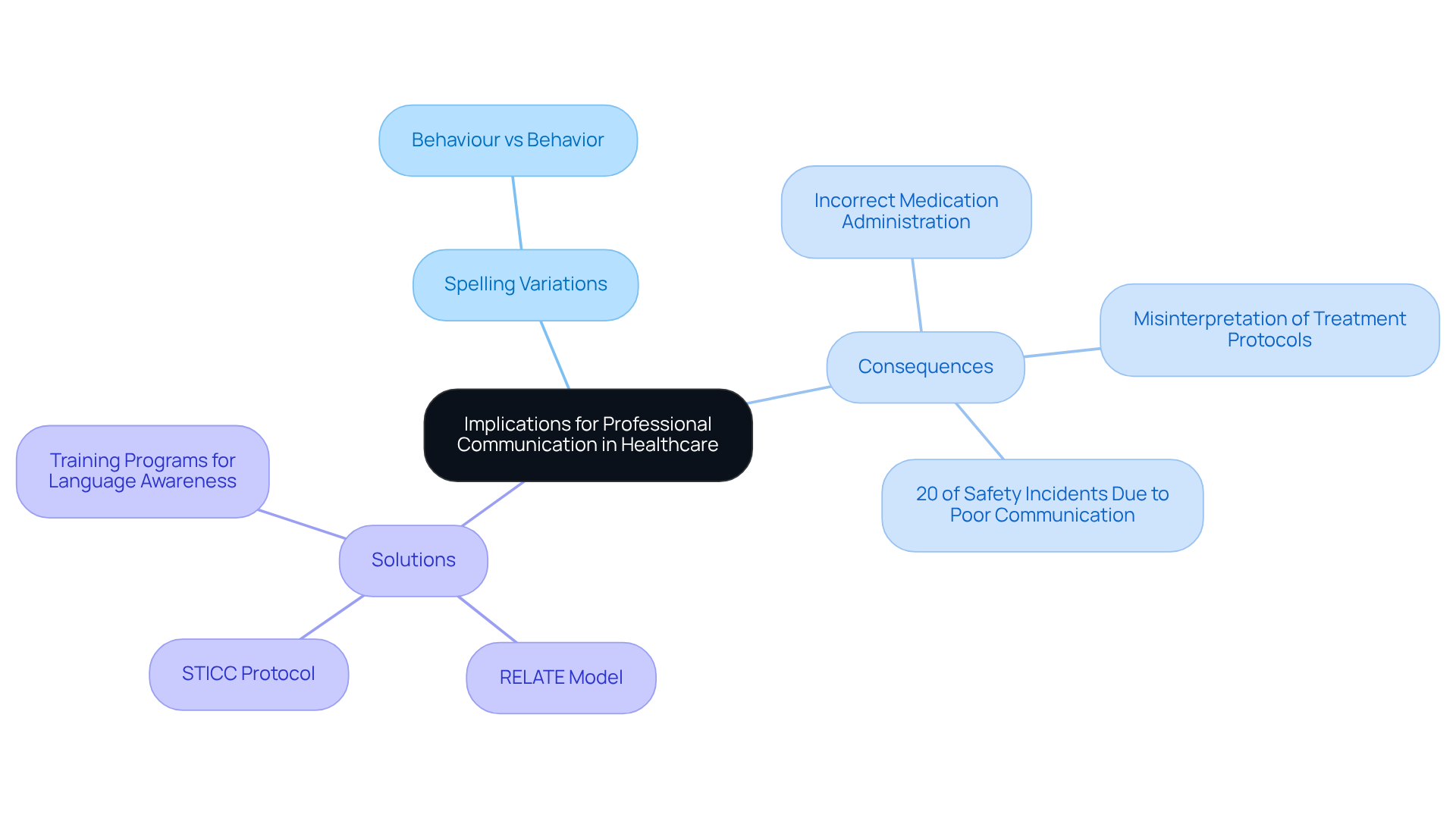
The implications of are significant, extending beyond mere academic curiosity to tangible consequences for client care. Misunderstandings stemming from language differences can result in serious errors, such as incorrect medication administration or misinterpretation of treatment protocols. For instance, if a British medical provider records a person's 'behaviour' in a report aimed at an American audience, the difference between 'behavior vs behaviour' could lead to confusion and miscommunication.
In multicultural healthcare environments, professionals must be acutely aware of these differences to promote effective collaboration and interaction. Statistics reveal that inadequate communication directly contributes to approximately 20% of safety incidents among clinical personnel, underscoring the urgency of addressing these issues.
Implementing training programs that focus on language awareness, such as the RELATE model or the STICC Protocol, can significantly enhance team dynamics and improve patient outcomes. Such initiatives ensure that all team members are synchronized on terminology and documentation standards, ultimately fostering a safer and more efficient medical environment.
As James Woodson, MD, emphasizes, "Patients’ lives often rely on swift and precise information sharing and cooperation among medical professionals.
Cultural factors significantly influence language usage in medical environments, shaping the understanding of behavior and interaction styles. For instance, some cultures favor direct communication, while others may lean towards a more indirect approach. Recognizing these cultural subtleties is vital for medical professionals aiming to establish trust and connection with individuals.
Furthermore, variations in terminology, such as 'behavior' vs 'behaviour', can convey distinct connotations across cultural contexts, impacting how medical messages are interpreted. Training medical personnel in enhances interaction effectiveness, leading to improved client engagements and superior health outcomes.
As cultural competence educators have noted, understanding different interaction styles is essential for fostering meaningful relationships with individuals from diverse backgrounds. Alarmingly, statistics indicate that one in five Americans seeking medical services encounters difficulties in interacting with doctors, with 33% of Hispanics facing similar challenges. Additionally, 23 states mandate some form of cultural competence training for Medicaid plans, highlighting the regulatory significance of such education.
As Selvedina Osmancevic asserts, 'Education and training can improve the level of nurses' cultural competence; therefore, they should be offered as continuing education for nurses.

Healthcare employers can significantly enhance interaction and safety for individuals by implementing standardized terminology guidelines. These guidelines ensure uniformity in documentation and communication across teams, which is crucial in a diverse healthcare environment.
Have you considered the implications of inconsistent communication on patient care?
Training staff in equips them with essential skills to effectively engage with individuals from various backgrounds. Furthermore, hiring bilingual personnel or utilizing expert translation services effectively bridges gaps in understanding, particularly for individuals who may not speak the primary language of the facility.
Regular evaluations and revisions of interaction protocols are essential to remain aligned with evolving language trends, ensuring that all team members share a comprehensive understanding of terminology.
By prioritizing clear and effective communication, healthcare organizations not only enhance patient satisfaction and safety but also contribute to improved health outcomes.
Are you ready to take actionable steps to elevate your team's communication standards?
Understanding the distinctions between 'behavior' and 'behaviour' is vital for healthcare professionals navigating the complexities of American and British English. These seemingly minor spelling differences carry significant implications for communication in medical contexts, where precision and clarity are paramount. As healthcare becomes increasingly globalized, recognizing and adapting to these linguistic variations is essential to ensure effective patient care and professional interactions.
Throughout the article, key points have highlighted the critical nature of language awareness in healthcare settings. From the potential for misunderstandings in clinical documentation to the impact of cultural factors on communication styles, it is clear that healthcare employers must prioritize training and standardization. Implementing best practices, such as uniform terminology guidelines and cultural competence training, can mitigate risks and enhance collaboration among diverse teams.
Ultimately, the significance of clear communication in healthcare cannot be overstated. By addressing the nuances of language and fostering an environment of understanding, healthcare organizations can improve patient outcomes and safety. Taking actionable steps to enhance communication standards is not just beneficial—it's essential for delivering high-quality care in today's interconnected world.
What are the main differences between American English and British English?
The main differences include variations in spelling, vocabulary, and usage. For example, 'color' in American English is spelled 'colour' in British English.
How can spelling differences impact medical contexts?
Spelling differences can lead to misunderstandings in medical documentation, which may affect care outcomes. For instance, 'behavior' in American English and 'behaviour' in British English could cause confusion if not properly addressed.
What are some examples of spelling variations in American and British English?
Examples include 'color' vs. 'colour' and 'behavior' vs. 'behaviour.' These variations reflect regional language preferences and can influence perceptions of professionalism in medical settings.
Why is it important to be aware of linguistic differences in healthcare?
Awareness of linguistic differences is crucial to ensure clarity and effectiveness in patient care, especially in a globalized medical environment where communication barriers may exacerbate health issues.
How can medical professionals navigate communication challenges arising from language differences?
Integrating insights from linguistics specialists can help illuminate the obstacles faced by medical professionals in managing these communication differences, ultimately enhancing patient outcomes.
What impact do communication barriers have on low-income Americans?
Low-income Americans face heightened risks of health issues, such as diabetes and hypertension, which can be exacerbated by communication barriers stemming from linguistic differences.
Our expert recruitment strategies and AI-driven sourcing ensure that you receive top-notch candidates quickly, without compromising on quality. Whether you’re looking for BCBAs, Clinical Directors, or RBTs, we’ve got you covered.