October 17, 2025

This article addresses the significant challenges and compliance requirements in ABA billing, underscoring the critical need for accurate documentation and a thorough understanding of payer-specific guidelines. By providing a comprehensive overview of the billing cycle, it highlights common obstacles such as claim denials and eligibility issues. Furthermore, it presents effective strategies to enhance compliance, ultimately ensuring successful reimbursement for ABA therapy services.
Are you aware of the complexities involved in ABA billing? This knowledge is essential for navigating the landscape and optimizing your practice's revenue cycle.
Navigating the intricacies of ABA billing can be a daunting task for healthcare providers, particularly as regulations and coding practices continue to evolve.
With the demand for Applied Behavior Analysis therapy on the rise, the complexity of ensuring compliance and maximizing reimbursement simultaneously increases.
This article explores essential steps and best practices necessary to master ABA billing, addressing common challenges and offering practical solutions.
How can providers streamline their billing processes effectively while adapting to the latest industry changes and minimizing claim denials?
ABA billing is a crucial process that involves submitting claims to insurance companies for reimbursement of services rendered in Applied Behavior Analysis (ABA) therapy. A vital component of this process is the use of Current Procedural Terminology (CPT) codes—standardized codes that accurately describe the services provided. Mastery of the latest CPT codes is essential for precise invoicing, particularly with the introduction of 270 new codes and the removal of 112 outdated codes in 2025. These updates enhance clarity and align financial practices with real-time care experiences, reflecting the unique needs of each patient. Given the heightened scrutiny from payers, providers must promptly update their invoicing and record-keeping strategies.
Understanding the diverse types of payers—such as —and their specific requirements is critical for successful billing. Each payer may have distinct records and authorization processes, making it imperative to stay informed about their guidelines.
Accurate and comprehensive records are essential to substantiate claims and ensure adherence to payer requirements. This includes maintaining HIPAA-secure records for a minimum of seven years and ensuring that all services are documented in real-time. Inadequate records are a leading cause of claim denials in ABA therapy, with initial denial rates ranging from 15% to 30%. As the ABA Coding Coalition states, 'The simplest method to safeguard your revenue is to ensure compliance with records.'
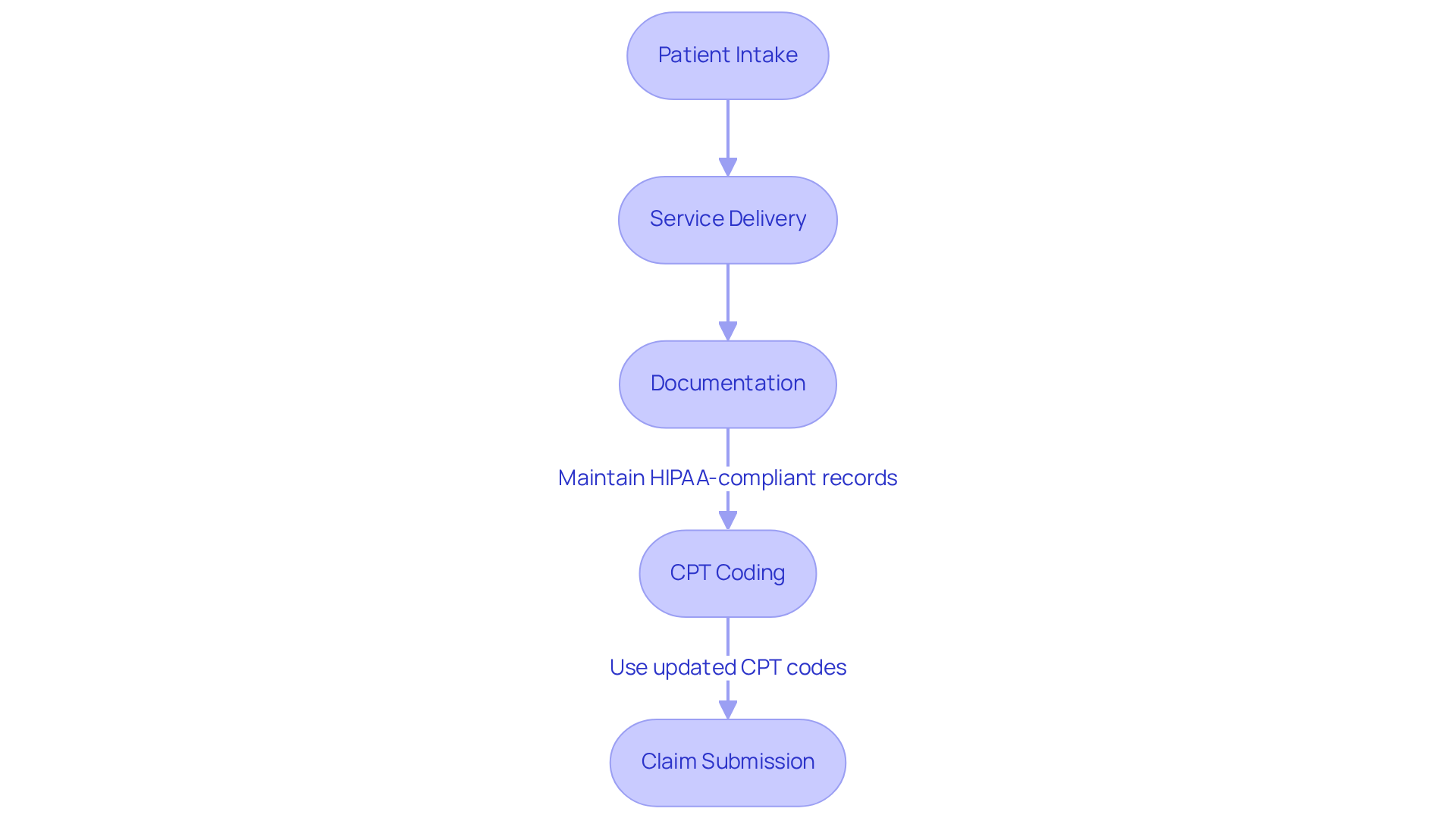
Familiarity with the payment cycle is also paramount. This cycle encompasses patient intake, service delivery, documentation, coding, and claim submission. By mastering these components, providers can navigate the complexities of ABA billing more effectively.
As the landscape of ABA therapy evolves, staying informed about the latest trends in ABA billing, CPT codes, and payment practices is essential for ensuring compliance and maximizing reimbursement. Regular training sessions and technology solutions, such as TherapyPM, which provides training modules and support documentation to assist staff in effectively utilizing new ABA CPT codes, can streamline these processes, ultimately enhancing the financial health of ABA practices. Furthermore, the temporary telehealth coverage extension until 2025 allows for ongoing remote supervision and treatment options, further influencing payment practices.
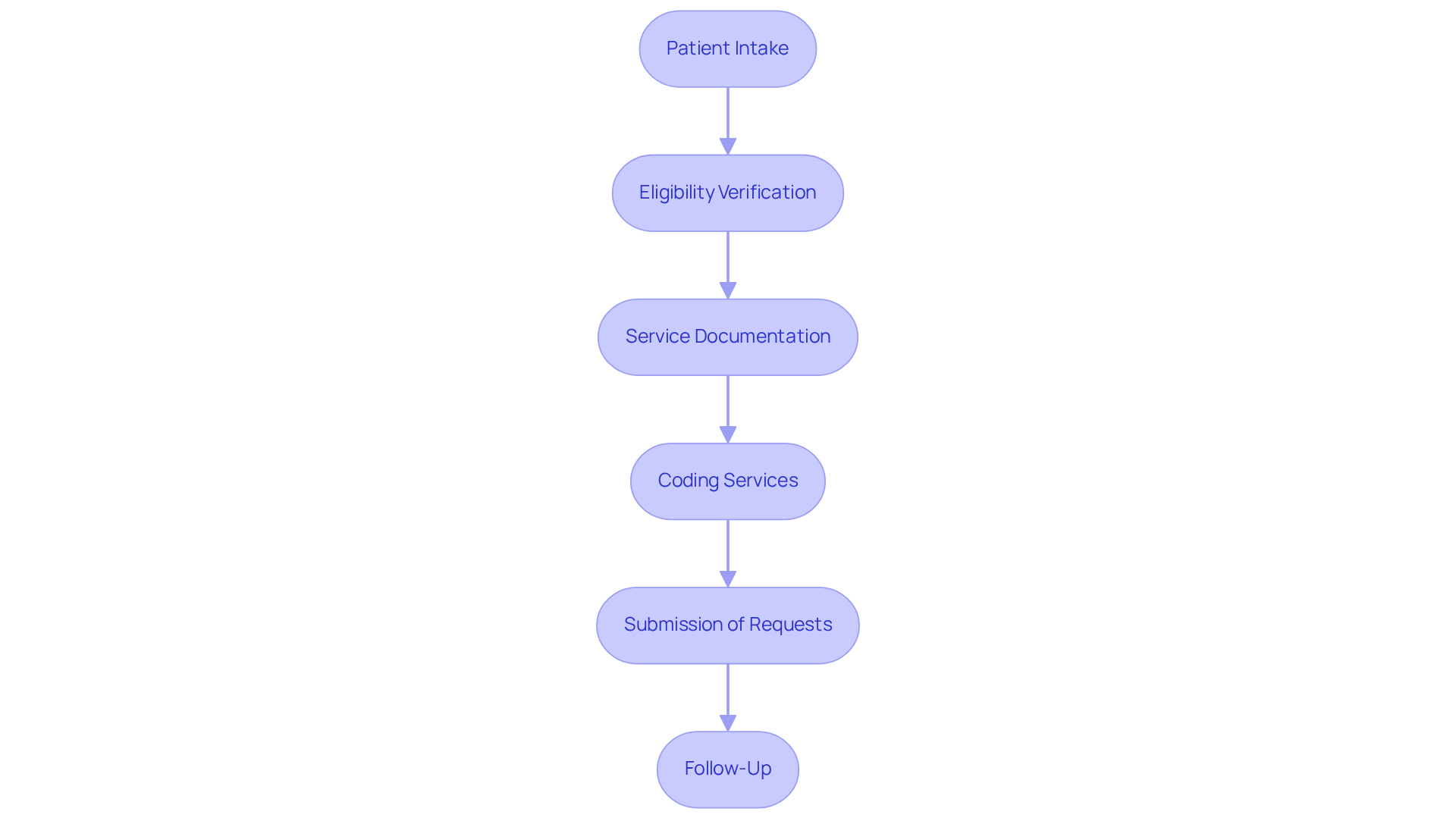
The aba billing cycle comprises several critical steps that ensure efficient processing and reimbursement. Did you know that roughly 27% of requests are rejected due to problems associated with patient registration and eligibility verification? This statistic underscores the importance of the initial phase of the billing cycle.
By diligently following these steps, healthcare providers can simplify the aba billing process and increase the chances of successful reimbursements, ultimately resulting in better financial outcomes. Moreover, consider this: it costs an average of $25 to revise a single denied claim. This highlights the significance of precision in the invoicing process.
Common challenges in ABA billing include:
By proactively tackling these challenges, you can reduce interruptions in your invoicing workflow and improve your practice's financial well-being.

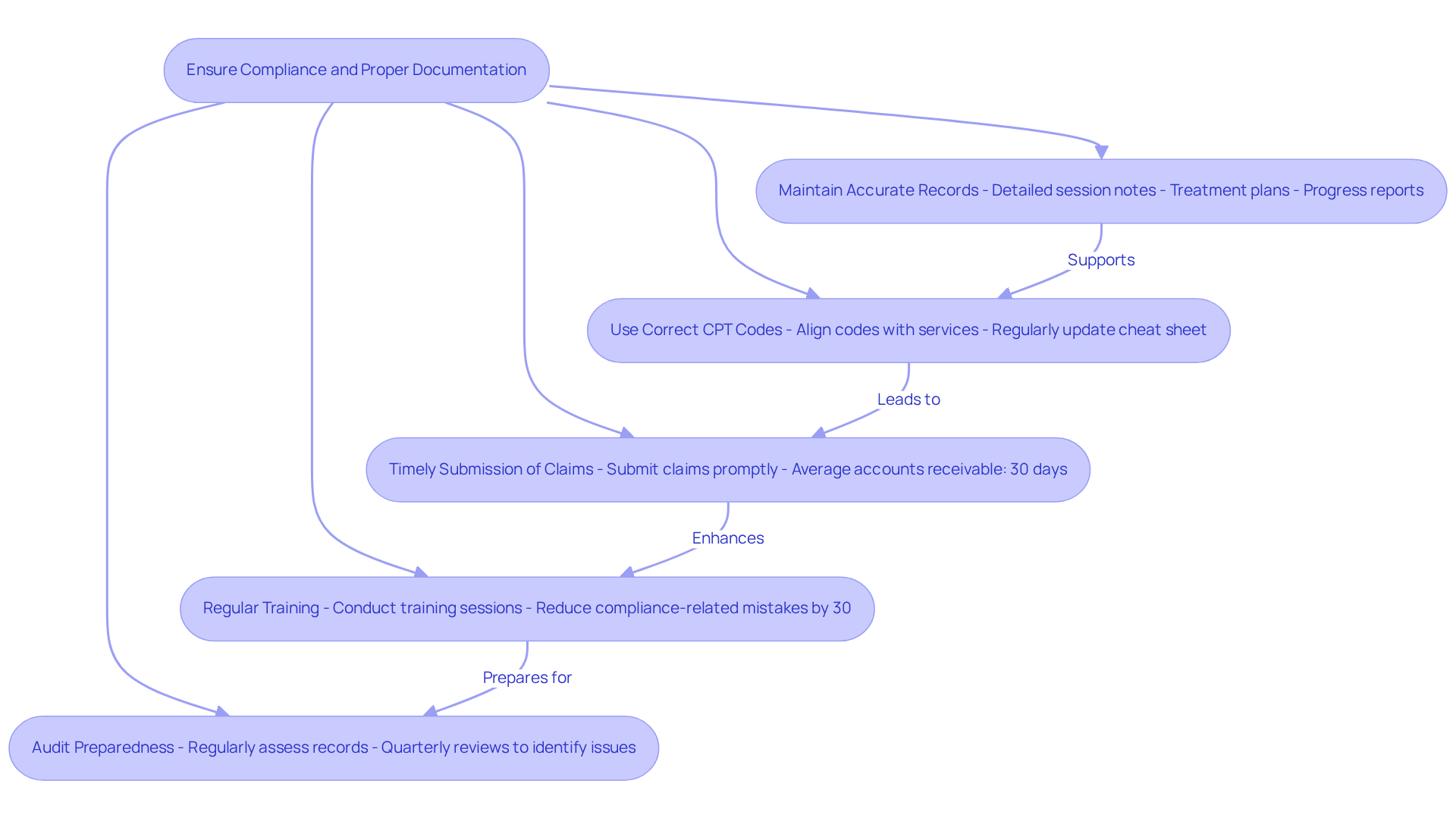
To ensure compliance and proper documentation in ABA billing:
By prioritizing compliance and documentation, practices can safeguard against penalties and enhance the efficiency of their ABA billing processes. As Kenneth Jeremiah, RCM expert at Plutus Health, states, "The financial implications of unresolved denials are substantial." Utilizing analytics tools can further assist organizations in identifying patterns and improving compliance, as highlighted in case studies on reducing health insurance claim denials.
Mastering ABA billing is essential for ensuring that providers can effectively navigate the complexities of reimbursement and compliance. The intricacies involved—from understanding CPT codes to managing payer requirements—underscore the necessity for diligence and attention to detail in the billing process. As the landscape of ABA therapy continues to evolve, staying informed and adapting to changes is critical for financial sustainability.
The article highlighted several key components of the ABA billing process, including:
By following a structured approach—starting from patient intake to timely claim submission—providers can significantly enhance their chances of successful reimbursement. Additionally, maintaining compliance through regular training and audits can mitigate risks associated with billing errors.
Ultimately, the significance of effective ABA billing cannot be overstated. It not only impacts the financial health of practices but also ensures that patients receive the necessary care without interruption. By implementing best practices and remaining proactive in addressing challenges, providers can secure their revenue streams and continue to deliver high-quality services in the field of Applied Behavior Analysis. Embracing these strategies will enhance operational efficiency and contribute to the overall success of ABA therapy practices in 2025 and beyond.
What is ABA billing?
ABA billing is the process of submitting claims to insurance companies for reimbursement of services rendered in Applied Behavior Analysis (ABA) therapy.
Why are CPT codes important in ABA billing?
CPT codes are standardized codes that accurately describe the services provided in ABA therapy. Mastery of the latest CPT codes is essential for precise invoicing, especially with updates that introduce 270 new codes and remove 112 outdated codes in 2025.
What impact do the updates to CPT codes have on ABA billing?
The updates enhance clarity and align financial practices with real-time care experiences, reflecting the unique needs of each patient, and providers must promptly update their invoicing and record-keeping strategies to comply.
What types of payers are involved in ABA billing?
The main types of payers include private insurance and Medicaid, each with specific requirements and distinct records and authorization processes.
Why is maintaining accurate records crucial in ABA billing?
Accurate and comprehensive records are essential to substantiate claims and ensure adherence to payer requirements. Inadequate records can lead to claim denials, which have initial denial rates ranging from 15% to 30%.
How long should records be maintained in ABA therapy?
Records should be maintained in a HIPAA-secure manner for a minimum of seven years.
What does the payment cycle in ABA billing include?
The payment cycle encompasses patient intake, service delivery, documentation, coding, and claim submission.
How can providers stay informed about ABA billing practices?
Providers can stay informed by participating in regular training sessions and utilizing technology solutions, such as TherapyPM, which offers training modules and support documentation for effective use of new ABA CPT codes.
What is the significance of the temporary telehealth coverage extension until 2025?
The temporary telehealth coverage extension allows for ongoing remote supervision and treatment options, which further influences payment practices in ABA therapy.
Our expert recruitment strategies and AI-driven sourcing ensure that you receive top-notch candidates quickly, without compromising on quality. Whether you’re looking for BCBAs, Clinical Directors, or RBTs, we’ve got you covered.